- 5th February 2026
Breast cancer is still more common after 50, but cases in younger women are increasing, and early action can save lives.
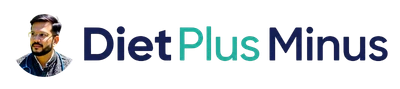
Many women still believe breast cancer is mostly a disease of older age. That belief is understandable, but it is no longer complete. Newer data shows a clear rise in diagnoses among younger women, especially those below 50. The American Cancer Society reports that incidence increased overall by about 1.0% per year in the recent decade, but the increase was steeper in women younger than 50 at 1.4% per year. This is exactly why awareness in your 20s and 30s is not overthinking. It is smart prevention.
A large JAMA Network Open analysis of women aged 20 to 49 also found an increase in breast cancer incidence over time, with important subtype and age-pattern insights. In simple words, younger-age breast cancer is not just a social media fear topic. It is a measurable clinical trend.
At Dr. Pankaj Kumar Medical and Lifestyle Clinic, the practical goal is to help women act early, avoid panic, and reduce delays. Early detection gives more treatment options, lower treatment burden, and better outcomes.
What does “rising under 40” actually mean
Rising risk does not mean every young woman is likely to get breast cancer. It means the number of cases in younger age groups is moving upward compared with previous years. So your response should be balanced: do not live in fear, but do not ignore persistent warning signs.
Another point to understand is subtype behavior. A large share of the recent rise appears in hormone receptor related patterns, especially estrogen receptor positive disease in many datasets. This matters because hormones, metabolism, and long-term lifestyle exposures may influence risk more than we previously appreciated.
Why are younger women seeing more breast cancer
1) Metabolic stress is increasing early in life
Today many women face insulin resistance, central weight gain, chronic stress, short sleep, and irregular meal timing much earlier than before. These changes can promote persistent low-grade inflammation and hormonal imbalance. Over years, that internal environment may support abnormal cell behavior. This does not prove a single direct cause, but it is one major biological pathway clinicians track closely.
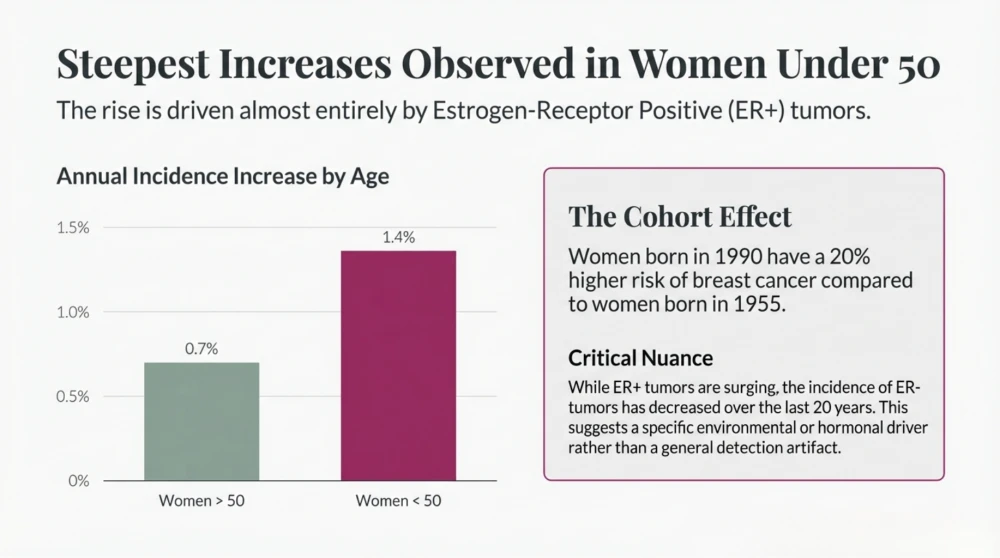
2) Long sitting hours are not harmless
Modern life means long desk time, commuting, laptop work, and late-night scrolling. Even women who exercise for 30 to 40 minutes can still be highly sedentary for the remaining day. Your body needs frequent movement breaks, not only one workout session. When sitting is prolonged and uninterrupted, metabolic flexibility worsens, and that can affect long-term disease risk.
3) Ultra-processed food load is becoming routine
Packaged foods are convenient, affordable, and everywhere. But when a large part of daily calories comes from ultra-processed foods, diet quality drops. Fiber falls, protein quality may be poor, sodium and sugar increase, and energy density rises. Over time this may worsen adiposity, insulin resistance, and inflammation, all relevant to long-term cancer risk.
4) Endocrine-disrupting chemical exposure is under serious review
Scientists are actively studying endocrine-disrupting chemicals (EDCs), found in some plastics, packaging materials, and personal care products. These compounds can interfere with hormone pathways. A recent Nature Reviews Cancer commentary highlights concern that chronic cumulative EDC exposure may contribute to early-onset estrogen receptor-positive breast cancer biology. This is an evolving area, but important enough to follow closely.
5) Reproductive timeline and life-stage biology also matter
Age at first period, pregnancy timing, postpartum remodeling, breastfeeding history, and ovarian hormonal patterns can all influence risk. This is why two women with similar lifestyles can still have different risk profiles. Breast cancer risk is multifactorial, and your personal history deserves individual review.
Symptoms younger women should never ignore
One common mistake is assuming every breast change is “hormonal” and will settle after periods. Some changes do settle, but persistent signs must be assessed. If any of the following last more than 2 to 4 weeks, get examined:
- New lump in breast or underarm
- One-sided persistent heaviness or discomfort
- Skin dimpling or orange-peel-like texture
- Localized redness, thickening, or swelling
- New nipple inversion, crusting, or spontaneous discharge
- Visible asymmetry that is new and persistent
Most lumps are not cancer, especially in younger age groups, but only proper evaluation can confirm safety. “Wait and watch for months” is not a wise strategy when signs persist.
Why diagnosis may get delayed in younger women
Dense breast tissue
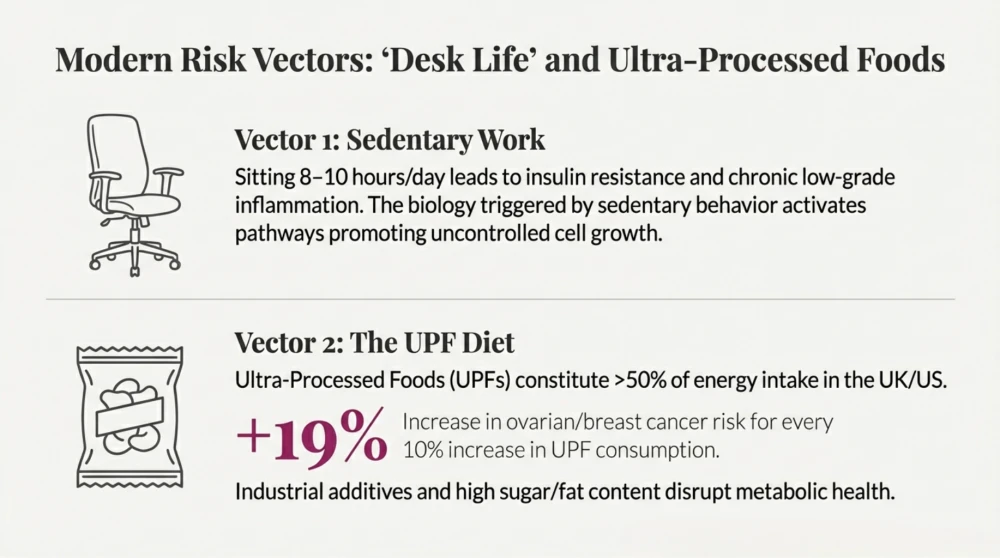
Younger women often have denser breast tissue, which can make interpretation more challenging in some imaging contexts. This is one reason symptom-led evaluation remains very important before routine screening age.
Low perceived risk
Many women and families still think “I am too young for breast cancer,” which delays first consultation. Delay is often due to reassurance by age, not by proper examination.
Busy life stage
Women in their 20s and 30s are often managing career pressure, marriage, childcare, and family responsibilities. Health complaints are postponed until symptoms become obvious.
Who should be extra careful
Every woman should practice breast awareness, but some profiles need earlier and tighter follow-up:
- Strong family history of breast or ovarian cancer
- Known BRCA1, BRCA2, or other high-risk mutation pattern in family
- Previous high-dose chest radiation at young age
- Prior high-risk biopsy findings (as advised by specialist)
- Obesity, inactivity, smoking, regular alcohol intake, and chronic sleep debt
If you fall in a higher-risk group, screening and prevention should be personalized. One generic rule does not fit everyone.
Screening: what to do and when
For average-risk women, the USPSTF recommends mammography every 2 years from age 40 to 74. If you are younger than 40 and symptomatic, do not wait for screening age. Symptom-led clinical evaluation should be done now.
If you have high-risk history, discuss earlier risk-based screening with your doctor. Depending on your profile, your plan may include targeted imaging and specialist referral before 40.
A practical prevention plan for general adult women
1) Protect your metabolic health
Keep waist circumference and body fat in a healthy range. Build muscle through resistance training 2 to 3 times per week. Add brisk walking most days. Small, consistent habits work better than extreme short-term diets.
2) Break sitting every 30 to 40 minutes
Stand, stretch, climb stairs, or walk for 3 to 5 minutes. These micro-breaks improve insulin response and reduce sedentary load.
3) Upgrade food quality
Use a simple plate rule: half vegetables, one-quarter quality protein, one-quarter whole grains or millets. Keep ultra-processed foods as occasional, not daily staples.
4) Sleep 7 to 8 hours regularly
Sleep is not optional recovery. Chronic sleep restriction can worsen appetite hormones, insulin resistance, mood, and inflammation.
5) Limit alcohol and avoid tobacco completely
Alcohol intake is linked with breast cancer risk. There is no health gain in smoking. Quitting helps risk reduction across multiple diseases.
6) Practice monthly breast self-awareness
You do not need fear-driven overchecking. You need familiarity with your own normal so new persistent changes are recognized early.
7) Get timely clinical assessment
Any change that persists beyond a cycle needs a doctor review. Early check is always easier than late intervention.
Common myths that delay diagnosis
“I am young, so it cannot be cancer”
Wrong. Risk is lower than older age, but not zero.
“If there is no pain, it is not serious”
Wrong. Many early breast cancers are painless.
“I exercise, so I am fully protected”
Exercise helps a lot, but it does not erase all risk. You still need sleep, nutrition quality, reduced sedentary time, and symptom vigilance.
“Family history is negative, so I am safe”
Family history helps risk prediction, but many breast cancer cases occur without a known family history.
When to consult urgently
- A hard or enlarging lump
- Bloody nipple discharge
- Rapid breast skin change, redness, or edema
- New unilateral nipple inversion with other local signs
- Persistent underarm node swelling
Do not self-diagnose online for weeks. Fast evaluation reduces anxiety and improves outcomes.
Medical disclaimer
This content is educational and does not replace personal medical advice, diagnosis, or treatment. For persistent symptoms or individualized risk planning, consult a qualified clinician.