- 9th February 2026
Table of Contents
- What these ads mean for real patients
- 1) Why the ad boom matters clinically
- 2) Branded vs compounded GLP-1: where patients get confused
- 3) Price and access are changing quickly
- 4) The biggest gap: people start treatment, then stop too early
- 5) What GLP-1 drugs can realistically do
- 6) The diet doctor’s core framework for weight loss on GLP-1
- A) Protein-first structure to protect muscle
- B) Fiber and volume to stabilize appetite
- C) Carbohydrate quality over carbohydrate fear
- D) Hydration and electrolytes matter more than patients expect
- E) Meal timing and pace
- 7) Weight management beyond injections
- 8) Who needs extra caution before starting GLP-1 therapy
- 9) The real takeaway from Super Bowl GLP-1 advertising
- Key points
What these ads mean for real patients
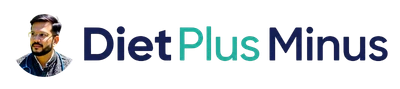
When weight-loss medicines reach the Super Bowl, it tells us one thing clearly: obesity care has moved from clinic rooms to mainstream conversation. In 2026, GLP-1 therapies appeared in high-visibility ad spots, including campaigns linked with major telehealth brands and celebrities. Reuters also reported this shift as a defining health-business storyline around the game.
That visibility has one big advantage: it reduces shame. More people now see obesity as a medical condition, not a character flaw. But it also creates confusion. Ads are designed to sell attention, not deliver individualized medical decisions. So if you are a patient, or a doctor counseling patients, the right response is neither blind excitement nor blanket rejection. The right response is clinical clarity.
This blog breaks down the real picture: what GLP-1 drugs can do, where risks are underestimated, why discontinuation happens, and why diet structure is the difference between temporary weight loss and durable weight management.
1) Why the ad boom matters clinically
Super Bowl advertising reaches a mass audience. That makes it a powerful stigma breaker, especially in obesity, where many people delay treatment because of judgment. Seeing obesity discussed openly can improve health-seeking behavior. At the same time, ad messaging often compresses a complex medical journey into a simple before-after narrative.
In real practice, obesity treatment is not a one-variable problem. It is a chronic metabolic condition influenced by appetite regulation, insulin resistance, sleep debt, stress load, food environment, muscle mass, movement patterns, and medication adherence. A drug can help with appetite and satiety, but it cannot independently fix all of these.
That is where many patients feel “misled” even when the medicine itself is effective. The expectation was “injection equals lifelong results.” The clinical reality is “medicine plus structured behavior plus follow-up equals sustainable outcomes.”
2) Branded vs compounded GLP-1: where patients get confused
One of the biggest confusion points in public discourse is the difference between FDA-approved branded medications and compounded versions.
The FDA has repeatedly warned about risks with unapproved compounded GLP-1 products, including dosing errors, quality concerns, and recent alerts about fraudulent products with false labels. The agency also announced enforcement actions against misleading promotional claims around non-approved compounded GLP-1s.
This does not mean every compounding situation is automatically unsafe. Compounding has a legitimate role in select circumstances. But for the average patient, the key point is simple: unapproved compounded products do not go through the same premarket evidence and quality pathway as approved branded drugs. So safety assurance is not equivalent.
As clinicians, we should explain this without fear messaging:
- Ask patients exactly what product they are using.
- Confirm source and prescription details.
- Review dosing method, concentration, and syringe technique.
- Screen for adverse effects early.
A calm safety-first conversation prevents harm better than blame.
3) Price and access are changing quickly
Historically, high monthly prices pushed many patients toward risky alternatives. In early February 2026, policy announcements and direct-to-consumer pricing channels (including TrumpRx-related announcements/pages) claimed substantially lower monthly prices for some GLP-1 options, with promotional entry pricing in selected doses.
For patients, lower prices can be a major positive because affordability strongly affects continuity. But two cautions are essential:
- Promotional prices are often dose- and duration-specific.
- Total treatment cost includes follow-up, labs, nutrition support, and long-term maintenance strategy.
So affordability is improving, but continuity still requires planning. A patient who can start but cannot sustain care may regain weight rapidly and feel discouraged.
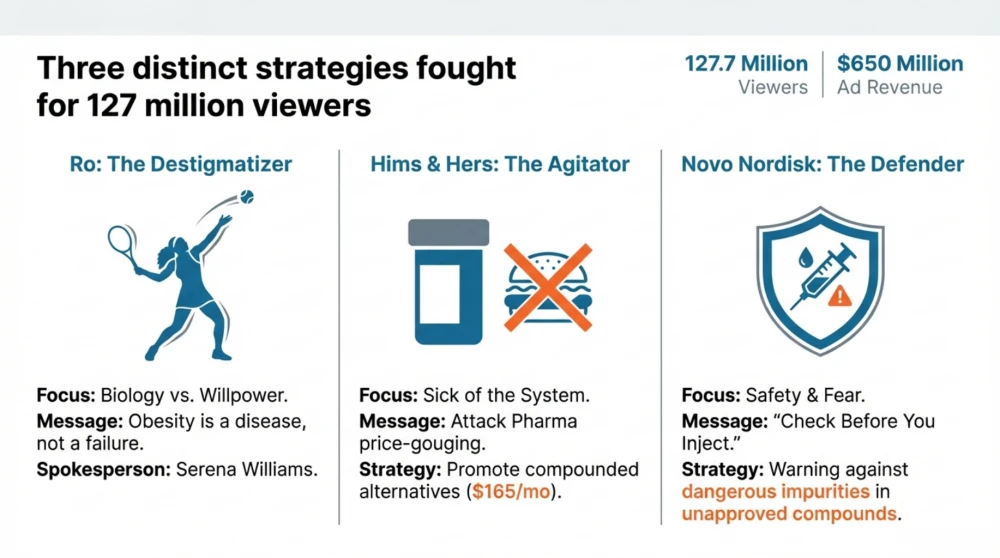
4) The biggest gap: people start treatment, then stop too early
In clinic reality, early discontinuation is common. Reasons include:
- nausea, fullness, reflux, constipation, or loose stools
- unrealistic weekly weight expectations
- dose escalation without proper counseling
- poor meal structure leading to fatigue and low protein intake
- cost or supply interruptions
- fear after social media side-effect stories
When patients stop abruptly without a transition plan, rebound hunger and old food patterns often return fast. This is where “the drug failed me” narratives begin, even when the true issue was incomplete treatment architecture.
5) What GLP-1 drugs can realistically do
GLP-1 receptor agonist therapies can reduce appetite, improve satiety, and in many patients support clinically meaningful weight reduction and glycemic benefits. That is real and valuable medicine.
But they do not:
- preserve muscle automatically
- teach food skills automatically
- fix emotional eating automatically
- normalize sleep automatically
- prevent regain automatically after discontinuation
So the correct message to patients is balanced:
These medicines are powerful tools, not standalone cures.
6) The diet doctor’s core framework for weight loss on GLP-1
A) Protein-first structure to protect muscle
When appetite drops on GLP-1, many patients under-eat protein and lose lean mass along with fat. That worsens weakness, hair fall, fatigue, and long-term regain risk.
Aim roughly 1.0-1.5 g protein/kg ideal body weight per day (individualize for kidney status, age, activity, comorbidities).
B) Fiber and volume to stabilize appetite
Use vegetables, salads, low-glycemic fruit, pulses, and whole-food textures. Fiber supports satiety and bowel regularity, especially when medication slows gastric emptying.
C) Carbohydrate quality over carbohydrate fear
You do not need “zero carb.” You need better carb timing and quality:
- choose minimally processed grains and pulses
- reduce sugar beverages, bakery foods, and ultra-processed snacks
- pair carbs with protein and fiber to flatten glucose spikes
D) Hydration and electrolytes matter more than patients expect
Low fluid intake worsens constipation, fatigue, headache, and nausea. Many side effects improve significantly when hydration is corrected.
E) Meal timing and pace
On GLP-1, fast eating causes discomfort. Encourage:
- smaller portions
- slower chewing
- stop at early satiety
- avoid lying down after meals if reflux-prone
7) Weight management beyond injections
Weight management cannot depend on injections alone, so I use a phased approach where the first stage focuses on symptom control and routine building, the next stage targets steady fat loss with higher protein quality and better food structure, and the final stage shifts to maintenance so results remain stable even with more flexibility. This phase-wise planning is important because calorie targets, protein needs, and behavior goals are different at each step.
I also emphasize movement as treatment, not as an optional add-on. If weight drops without resistance training and daily movement progression, muscle loss increases and regain risk becomes higher, so a practical combination of regular strength work and gradually improving step count is essential for preserving metabolism and long-term outcomes.
Sleep and stress are equally critical because poor sleep amplifies hunger and cravings, while chronic stress weakens consistency even in motivated patients. That is why close early follow-up matters: it helps us manage dose tolerance, bowel or reflux issues, protein adequacy, and adherence in real time, so small problems are corrected early before frustration leads to dropout.
8) Who needs extra caution before starting GLP-1 therapy
- personal or family history relevant to thyroid C-cell tumor warnings for certain GLP-1 agents
- pancreatitis history
- severe gastrointestinal disease or uncontrolled reflux/gastroparesis concerns
- pregnancy, lactation, or active conception planning
- eating disorder risk
- interacting medications and renal/hepatic context
Also verify medication source carefully. FDA communications have highlighted fraudulent and mislabeled compounded products, which can introduce avoidable safety risk.
9) The real takeaway from Super Bowl GLP-1 advertising
The ads are not the problem. The interpretation is the problem.
If mass advertising helps people seek care earlier, that is good. If it pushes rushed prescribing, unsafe sourcing, and unrealistic expectations, that is harmful. The solution is evidence-based clinical pathways where medication, nutrition, movement, and follow-up are integrated from day one.
For long-term success, think like this:
- Medicine starts momentum
- Diet and lifestyle build the engine
- Clinical follow-up keeps results stable
That is how we convert short-term weight loss into long-term metabolic health.
Key points
- GLP-1 therapies are effective tools, but not stand-alone cures.
- FDA has issued multiple warnings on risks tied to unapproved/fraudulent compounded GLP-1 products.
- Price accessibility appears to be improving in 2026 policy/market channels, but continuity still depends on full care planning.
- Early discontinuation is common when side effects and diet structure are not managed proactively.
- Protein-first meals, fiber, hydration, resistance training, and scheduled follow-up are the foundation of sustainable weight management.