- 7th February 2026
Walk into any pharmacy or scroll through any health app, and you will see the same promise everywhere: “Fix your gut with probiotics.” It sounds simple, reassuring, and modern. But if you have ever tried a probiotic and felt no change, you are not alone. The truth is more nuanced. Probiotics can be useful, sometimes very useful, but they are not a magic reset button for every digestive complaint.
A healthier way to think about probiotics is this: they are tools, not miracles. Like any medical or nutrition tool, results depend on the right match, the right dose, and the right situation. In this blog, I will break this down in plain language so you can make practical decisions without getting lost in marketing claims
First, what are probiotics in real terms?
Probiotics are live microorganisms that can provide health benefits when taken in adequate amounts. Most people describe them as “good bacteria,” which is fine for basic understanding, but it is incomplete. Different probiotic strains behave differently in the body. One strain may help with antibiotic-related diarrhea, while another may help with bloating in some people, and a third may do very little for your specific problem.
Your gut is not empty waiting to be “filled.” It is already a living ecosystem containing trillions of microbes. These microbes help digest food, train your immune system, produce useful compounds, and support the gut barrier. When this ecosystem gets disturbed, symptoms like gas, bloating, irregular motions, loose stools, or discomfort can appear. Probiotics may support recovery, but they do not replace everything that was lost, and they do not work like a permanent transplant for most people.
Why people get confused about probiotics
The biggest confusion comes from one assumption: if probiotics are good, then any probiotic should work. That is not how science works here. Benefits are strain-specific and condition-specific. This means you cannot choose only by brand name, price, or “billions of CFU” on the box and expect reliable results.
Many products are sold as if they solve everything from acidity to mood to skin glow in one capsule. Real outcomes are usually narrower. A probiotic that helps after antibiotics may not be the best one for constipation. A product that works for one person may not work for another because baseline gut composition, diet, sleep, stress, and medical history are different.
So the practical question is never “Which probiotic is best?” The better question is “Best probiotic for what?”
How probiotics actually help the gut
Let us simplify the mechanism without overselling it.
- One, probiotics can help by competing with harmful organisms for space and nutrients in the gut. Think of your gut lining as parking space. If helpful microbes occupy those spots, harmful organisms find less room to settle.
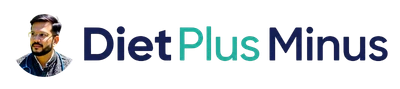
- Two, certain strains support the gut barrier. A stronger barrier means fewer irritants crossing into deeper tissues where they can trigger immune responses and inflammation.
- Three, probiotics can influence local immune signaling in the gut. They do not “boost immunity” in a dramatic superhero way, but they may help your immune system respond in a more balanced manner.
- Four, some strains help produce or support beneficial metabolites, including short-chain fatty acids, which nourish gut cells and support a healthier internal environment.
The key point is that these are supportive effects. Probiotics can improve the environment, but they are not stand-alone cures for all gut disease.
The strongest practical use: during and after antibiotics
If there is one area where probiotics make immediate clinical sense, it is this. Antibiotics are often necessary and life-saving, but they can also disturb normal gut flora. That is why many people get loose stools or abdominal upset during antibiotic treatment.
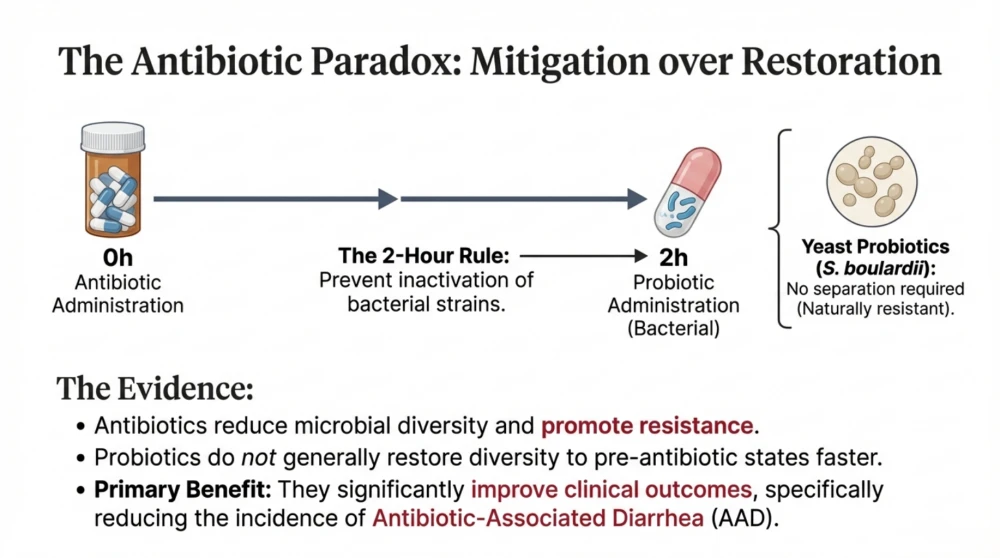
In this context, selected probiotics can reduce the risk or severity of antibiotic-associated diarrhea. Two names that are frequently used in this setting are Lactobacillus rhamnosus GG and Saccharomyces boulardii. Saccharomyces is a yeast, not a bacterium, and that matters because regular antibiotics target bacteria, not yeast.
Timing is important. If you are taking bacterial probiotics, keep a gap of around two hours from antibiotic doses so the antibiotic does not inactivate the probiotic immediately. Yeast-based probiotic timing is less affected by this issue. Continue for the antibiotic course and often for one to two weeks afterward, depending on symptoms and clinician advice.
What probiotics are doing here is not permanently replacing your original flora. They are acting like temporary stabilizers while your native ecosystem recovers.
Can probiotics help bloating, constipation, IBS, skin, and mood?
This is where expectations should be realistic.
- For bloating and irritable bowel syndrome type symptoms, some people improve, some do not. You may need a short, structured trial with a specific strain and clear symptom tracking. Randomly changing products every few days usually creates confusion, not results.
- For constipation, selected strains may improve stool frequency or consistency in some individuals. But if water intake is poor, fiber is too low, activity is minimal, and sleep is poor, probiotic benefits will be limited.
- For immunity, probiotics may reduce the frequency or duration of some minor infections in selected groups, but effects are usually moderate.
- For mood and stress, the gut-brain connection is real and fascinating, but this field is still evolving. Probiotics are not substitutes for mental health care, sleep recovery, movement, stress regulation, or proper treatment where needed.
- For skin, some early evidence is promising for specific indications, but broad claims like “all skin problems improve with probiotics” are not evidence-based.
In short, probiotics can support, but they do not replace fundamentals.
Who should be cautious before using probiotics
For most healthy adults, probiotics are generally safe, and side effects are usually mild, like temporary gas or bloating in the first few days.
However, caution is important in high-risk groups. This includes severely ill hospitalized patients, people with significant immune suppression, premature infants, and those with central venous catheters. In rare cases, live microorganisms can cause serious infection in vulnerable individuals. So self-prescribing without supervision is not wise in such situations.
If someone has major ongoing gut symptoms, unexplained weight loss, blood in stool, persistent fever, or severe abdominal pain, probiotics should not be the first or only response. Diagnosis comes first.
How to choose a probiotic without getting trapped by marketing
When you pick a product, read the label like a clinician, not like an advertisement.
Look for full strain identity, not just genus names. “Lactobacillus blend” is vague. A good label gives full strain information. Check whether the product indicates viability till expiry, not only at manufacturing. Follow storage guidance, because heat and humidity can reduce potency for some products.
Most importantly, choose based on your symptom goal. If your issue is post-antibiotic diarrhea, use evidence-backed strains for that purpose. If your issue is IBS-like bloating, choose a product studied for that context.
Do not combine three probiotics, two digestive enzymes, and multiple herbal powders at once. If everything changes together, you cannot know what helped and what caused side effects.
Best-use strategy
Start one product with a clear reason. Use it consistently for a defined trial, usually two to four weeks for non-acute symptoms. Track two or three symptom markers such as bloating score, stool frequency, urgency, or abdominal discomfort. If you see clear improvement, continue for the advised duration. If there is no meaningful change, reassess rather than increasing dose endlessly.
Also remember that probiotics work best when your routine supports them. Regular meal timing, enough hydration, adequate fiber, daily movement, and sufficient sleep are not optional add-ons. They are the base layer of gut recovery.
If you keep eating highly processed food, sleeping late, staying stressed, and remaining sedentary, a probiotic alone cannot override those pressures.
Food versus supplements: do you need both?
Not always. Fermented foods like curd and some traditional preparations can support gut diversity, especially when tolerated well. Whole foods rich in fiber help feed beneficial gut microbes over time. In many people, improving food quality and routine habits gives more durable results than capsules alone.
Supplements are useful when you need targeted support, such as after antibiotics, during specific symptom phases, or when diet alone is not enough. The smart approach is food-first with supplement support when indicated.
Symptoms you should not ignore
Please do not self-manage indefinitely with probiotics if you have blood in stool, persistent fever, dehydration, severe pain, repeated vomiting, or unexplained weight loss. These are warning signs and require medical evaluation.
If symptoms persist beyond a couple of weeks despite basic correction, it is time to investigate causes such as infection, inflammatory conditions, thyroid issues, food intolerances, medication effects, or other gastrointestinal disorders.
Key Points
Probiotics can help gut health, but they do not “heal everything.” They are most effective when used for the right indication, with the right strain, in the right person, for the right duration. They are supportive partners, not miracle cures.
If you remember just one line, remember this: strain matters more than hype, and routine matters more than capsules.
Use probiotics thoughtfully, pair them with food and lifestyle correction, and seek medical guidance when symptoms are persistent or severe. That is the evidence-based, practical, and safe way to improve gut health.